Author: Dr. Ayisha Anwar,(General Practitioner – WELLKINS Medical Centre)
This article delves into the specific dietary needs and considerations for individuals managing diabetes. It probably provides valuable information and guidance on how people with diabetes can make informed food choices, manage their blood sugar levels effectively, and adopt healthier eating habits.
Diabetes is a metabolic disorder characterized by high blood sugar (hyperglycemia) due to problems with insulin production, insulin action, or both.
Type 1 diabetes involves the body stopping insulin production, requiring external insulin. It’s usually caused by an autoimmune process.
Type 2 diabetes is a progressive disease with insulin resistance (cells don’t respond properly to insulin) and often insufficient insulin production.
Individuals with diabetes have a higher risk of serious complications like heart disease, stroke, kidney disease, eye problems, foot issues, erectile dysfunction, and nerve damage. Healthy eating and lifestyle changes are crucial for managing diabetes and reducing these risks.
Why Healthy Eating is Important:
Helps prevent or manage high blood sugar, high blood pressure, and unhealthy cholesterol levels, reducing hospitalizations.
- Early nutrition education after diagnosis is vital for implementing healthy habits.
- Ongoing nutrition and diabetes self-management education are important for long-term success.
Managing Type 2 Diabetes with Lifestyle:
Type 2 diabetes can be managed through diet and lifestyle changes. If blood glucose and A1c targets aren’t met within three months of lifestyle and nutrition management, medication should be considered.
Regular Meals:
- Eating three meals a day, including breakfast, is generally recommended for good blood sugar control.
- Meal timing and spacing should be individualized based on lifestyle and treatment goals
- Intermittent fasting may be considered by some, but requires careful planning and consideration of risks and medication adjustments.
Balanced Meals:
- A balanced meal includes a variety of vegetables, fruits, whole grains, and protein-rich foods.
- Breakfast should include protein along with carbohydrates.
Portion Sizes:
- Using hands can help estimate appropriate portion sizes:
*Fist: grains/starches or fruit
*Two handfuls: vegetables
*Palm and little finger thickness: meat, fish, poultry *Tip of the thumb: added fat
Snacks:
Not everyone with diabetes needs snacks.
They can be helpful when:
- Meals are 4-6 hours apart.
- Low blood sugar occurs without a snack.
- Increased physical activity leads to hypoglycemia risk.
- Evening snacks improve morning blood sugars.
- Snacks help with portion control at meals.
- Recommended snacks are high in fibre, include protein, and are low in added sugars and fats.
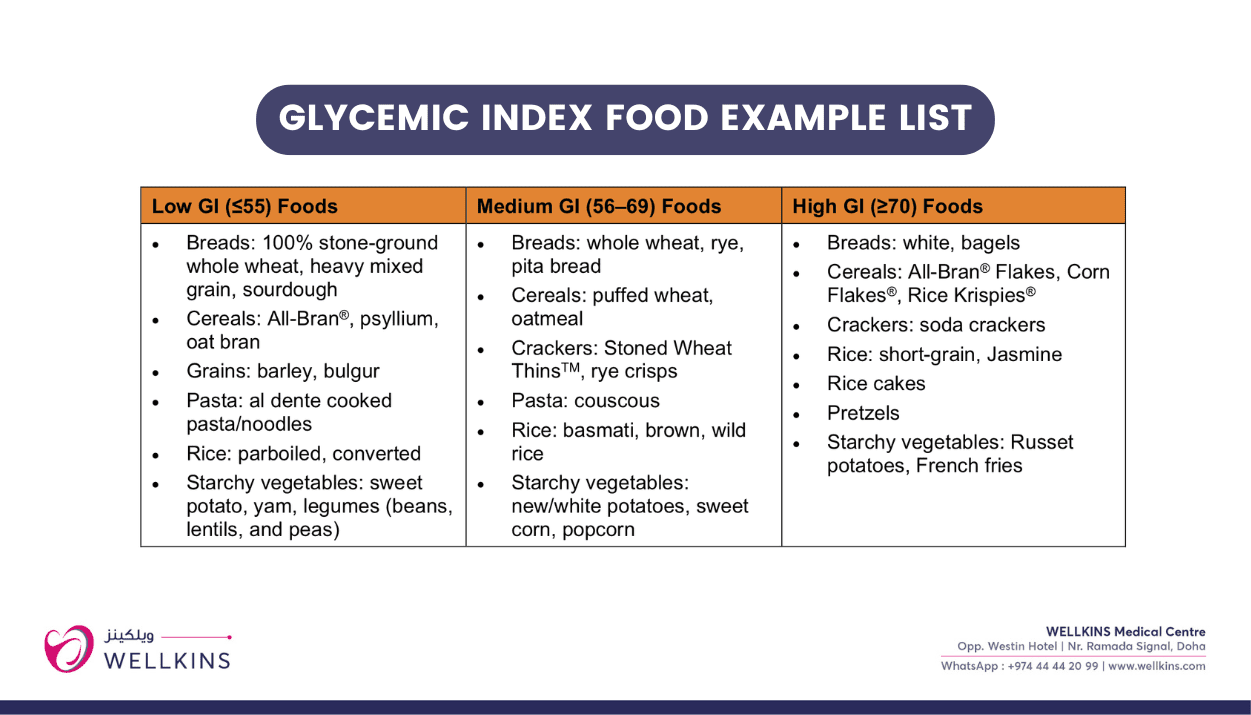
Glycemic Index (GI):
GI ranks carbohydrate-rich foods (1-100) based on how much they raise blood glucose.
- Low GI foods (≤55) cause a slower rise in blood sugar, while high GI foods (≥70) cause a rapid rise.
- Factors like fibre, protein, fat, carbohydrate type, acid content, processing, and cooking affect GI.
- Exchanging high GI foods for low GI options can help manage blood sugar.
- Education on GI should consider the patient’s interest and ability, as it’s a more complex concept.
- Serving size remains important even with low GI foods.
- Tips for using GI include incorporating vegetables, fruits, and milk, planning meals with medium and low GI grains, and limiting high GI foods. Examples of low, medium, and high GI foods are provided.
Sugar and Sugar Substitutes:
People with diabetes should limit free sugars (added sugars and sugars in honey, syrups, and fruit juices) to less than 5-10% of total daily energy. Recommended maximum daily amounts based on calorie intake are provided. High intake of sugar-sweetened beverages is linked to increased risk of hypertension and heart disease in people with diabetes. Sugar substitutes (artificial sweeteners, high-intensity sweeteners, and sugar alcohols) are safe in moderation below acceptable daily intake.
They can help reduce calorie intake and lower the glycemic response when replacing added sugars. -“Sugar-free” or “no sugar added” foods can still be high in fat and calories.
Sugar alcohols have little effect on blood glucose (2 kcal/g) but should be limited to ≤10 g/day to avoid gastrointestinal issues.
Dietary Patterns:
Several dietary patterns can aid blood sugar management and reduce cardiovascular risk, (emphasizing whole grains, vegetables, fruit, and limiting saturated fats, sugar, and sodium).
Mediterranean diet: Plant-based, rich in vegetables, fruits, legumes, nuts, seeds, whole grains, olive oil, moderate in dairy, fish, poultry, and red wine, low in red meat, added sugars, and processed foods. Shown to reduce cardiovascular events and improve blood sugar control.
Vegetarian diet: Excludes meat, fish, and poultry, emphasizes plant-based foods, typically lower GI, lower in saturated fat, and higher in fibre, aiding glucose and weight management and reducing cardiovascular risk.
DASH (Dietary Approaches to Stop Hypertension) diet: Emphasizes vegetables, fruits, lower-fat dairy, whole grains, poultry, fish, and nuts. Effective in lowering blood pressure and improving blood sugar control and cardiovascular risk factors.
Sodium intake should be limited to less than 2300 mg daily for the general population with diabetes, and closer to 2000 mg for those with hypertension.
Eating Out:
Restaurant meals are often higher in fat and sodium and have larger portion sizes.
Tips for healthy eating out include sharing meals, ordering half to go, avoiding fried foods, choosing balanced meals with vegetables, asking for leftovers, having a snack beforehand, considering salad as a starter, limiting eating out, and choosing sugar-free beverages.
Vitamins, Minerals, and Natural Health Products:
Most people with diabetes can meet their nutritional needs through a balanced diet. Routine supplementation is generally not needed, except for:
Folic Acid: Recommended for women of childbearing age (1.0 mg daily at least 3 months before conception, may decrease to 0.4 mg in the second trimester). A daily multivitamin is also suggested during pregnancy and lactation.
Vitamin D: Supplementation is necessary for most Albertans, including those with diabetes (400 IU daily for adults 19-50, 1000 IU daily for those 51+).
Vitamin B12: Long-term metformin use (>4 years at >1 gram daily) increases the risk of deficiency, and periodic testing is suggested for those with anemia or neuropathy. Supplementation may be needed.
Other supplements may be recommended in specific cases of deficiency or limited intake.
Meal replacements and specialty diabetes products are not required for blood sugar management. Weight:
Most individuals with type 2 diabetes have obesity, and its prevalence is increasing in type 1 diabetes.
Modest weight loss (5-10% of initial weight) can improve metabolic health in those with excess weight.
BMI and waist circumference (WC) are used to assess health risk, but BMI has limitations for individual targets. Elevated WC (≥102 cm for males, ≥88 cm for females; ethnic-specific measurements exist) indicates increased risk.
Focusing on positive, sustainable behavior changes is recommended over strict weight-based goals. “Best weight” is defined as the weight achieved while enjoying a healthy lifestyle, including enjoyable foods and exercise.
Physical Activity:
Regular physical activity reduces mortality in both type 1 and type 2 diabetes.
It improves blood sugar management in type 2 diabetes (and offers other benefits in type 1), increases cardiovascular fitness, improves lipid profile and blood pressure, helps maintain weight loss, and promotes bone and joint health and stress reduction.
Individuals should be evaluated for complications before starting an exercise program.
Those on insulin or secretagogues are at risk of hypoglycemia and may need medication or carbohydrate adjustments.
Both endurance (aerobic) and strength (resistance) exercises are recommended. Endurance activities should total 150 minutes/week, spread over at least three non-consecutive days. Strength training should be done 2-3 times per week. Supervised exercise programs tend to have better outcomes. Reducing sedentary time is also important.