Author: NIKITHA FERNANDEZ (Clinical Psychologist – WELLKINS Medical Centre)
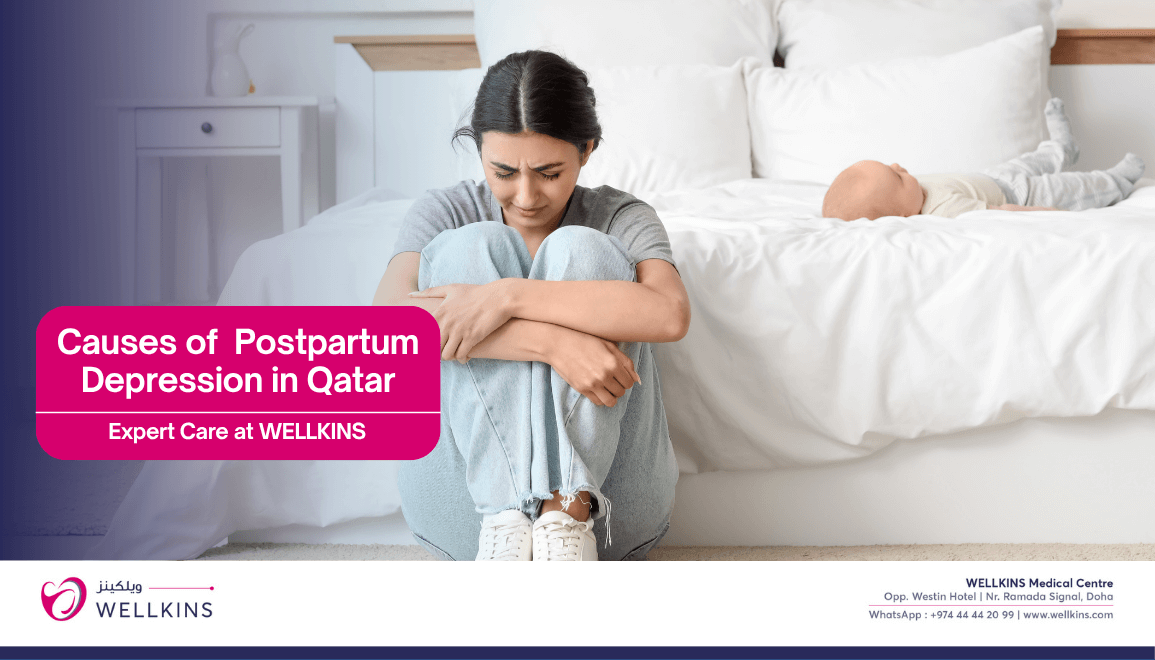
Welcoming a new baby is often imagined as a time of pure joy, love and excitement. Yet for many mothers, the reality is more complicated. The weeks and months after giving birth can bring unexpected waves of sadness, anxiety, and exhaustion. These feelings can be confusing, frightening, and often isolating. At Wellkins Medical Centre, we recognize that maternal well-being is as crucial as physical health. Postpartum depression (PPD) is more common than most people realize, and it is not a sign of weakness or failure it’s a real, treatable condition that affects mothers physically, emotionally and mentally.
PPD goes beyond the “baby blues,” which usually fade within a couple of weeks. It can linger, interfere with daily life and impact a mother’s ability to feel connected to her baby. The causes are complex, involving shifts in hormones, changes in brain chemistry, sleep deprivation, stress and the enormous emotional adjustment of becoming a parent. Many mothers feel overwhelmed by guilt or shame, worrying that they should be “happy” but aren’t.
It’s important to remember: you are not alone. Understanding PPD from its signs and risk factors to its impact on daily life can help mothers and families recognize when support is needed. Early help makes a difference and recovery is possible and ensuring mothers receive the understanding and care they deserve during this vulnerable time.
“It is observed that stress often presents as physical tension or racing thoughts, but in mothers experiencing Postpartum Depression (PPD), the distress is fundamentally different and requires clinical intervention. This is not simply fatigue or the transient ‘baby blues’ (sudden hormonal and chemical changes that take place in your body after childbirth); it is a powerful, persistent emotional disorder characterized by profound sadness, intrusive guilt, severe anxiety and, critically, an impaired ability to function or connect with the infant. PPD is a medical condition demanding specialized psychological care.”
What Causes Postpartum Depression?
Postpartum depression arises from a combination of biological, psychological and social factors. Biologically, the sudden dramatic drop in hormones like estrogen and progesterone after childbirth can profoundly affect brain chemistry and mood regulation. Psychologically, the intense pressure to be a “perfect” mother, coupled with the emotional trauma of childbirth or pre-existing mental health conditions, can increase vulnerability. Socially, factors such as sleep deprivation, lack of practical support, financial strain and relationship difficulties create an environment of chronic stress that can trigger or worsen depressive symptoms.
Hormonal Changes: After childbirth, levels of estrogen and progesterone drop rapidly, which can affect mood and emotional regulation.
Brain Chemistry: Neurotransmitters like serotonin and dopamine chemicals that influence mood, motivation and reward can become imbalanced, making it harder to cope with stress.
Sleep Disruption: Newborn care often means fragmented sleep, which can amplify feelings of irritability, sadness and anxiety.
Psychological Stress: The sudden shift in identity, pressures of caring for a newborn and societal expectations can weigh heavily on a new mother.
Life Circumstances: Limited social support, financial pressures, or a history of depression or trauma can increase vulnerability to PPD.
Recognizing the Signs
Postpartum depression can show up in many ways. Common symptoms include:
- Persistent sadness, emptiness, or tearfulness.
- Loss of interest or pleasure in things you once enjoyed.
- Fatigue, restlessness, or difficulty sleeping (beyond normal baby-related sleep loss).
- Anxiety, panic attacks, or constant worry.
- Feelings of guilt, shame, or inadequacy.
- Trouble bonding with the baby or feeling disconnected.
- Changes in appetite or weight.
- In severe cases, thoughts of self-harm or harming the baby.
If you notice these symptoms lasting more than two weeks, or if they are severe, it’s important to reach out for professional support.
Why Support Matters
Postpartum depression doesn’t just affect mothers it impacts partners, families and the baby’s development. Early intervention can make a significant difference:

- Therapy or counseling provides a safe space to talk and process emotions.
- Medication, if needed, can help restore chemical balance in the brain.
- Social support from family, friends, or parent groups helps mothers feel less
isolated. - Lifestyle adjustments, including rest, nutrition and gentle exercise, can improve
mood and resilience.
Neuroscience research also highlights the brain’s remarkable ability to adapt. Concepts like neuroplasticity the brain’s capacity to reorganize itself and neurogenesis the growth of new neurons suggest that with support, recovery and emotional balance are achievable. Practices such as mindfulness, gentle exercise, or even vagus nerve stimulation (under medical guidance) can positively influence stress responses and mood regulation.
Practical Steps for Mothers and Families
Acknowledge Your Feelings: Accept that struggling after childbirth is common and does not make you a bad mother.
Seek Help Early: Talk to your healthcare provider, therapist, or counselor. Early intervention improves outcomes.
Build a Support System: Lean on trusted family, friends, or support groups. Connection is crucial.
Prioritize Self-Care: Sleep, when possible, eat nourishing foods and allow small breaks for yourself.
Stay Informed: Understanding PPD reduces fear and self-blame. Knowledge supports recovery.

Postpartum depression is a journey no mother should face alone. At Wellkins Medical Centre, we are dedicated to supporting you through that journey. It is a medical condition, rooted in complex biological and emotional changes, but one that is fully treatable with the right support. Recognizing the signs, reaching out for help and leaning on family, friends and professionals can make the transition to motherhood less overwhelming and more hopeful.
Feeling lost, sad, or anxious after childbirth doesn’t make you weak; it makes you human. We want you to know that healing is possible. With understanding, expert care and timely intervention, the path to recovery is clear and life with your baby can become joyful again.
Postpartum depression is not just a clinical condition, it is a deeply personal and culturally shaped experience that deserves empathy, awareness and informed support. As we continue to challenge stigma and expand conversations around maternal mental health, it becomes crucial to understand how each woman’s social world, beliefs and expectations can influence her emotional recovery after childbirth. For readers who wish to explore this dimension further, I invite you to read my published research article, “Study of Cultural Factors Leading to Postpartum Depression in Women,” which is attached here:
Disclaimer: This blog is for informational purposes only and should not replace professional medical advice.